Simpson’s Paradox and Specialty Carve-Out Contracts: Risks for Health Insurers in Cost Analysis
Several studies show that the cost of carveouts varies up to 50% by network and system, even when adjusted for patient characteristics 1. How do you structure your carve-out contracts to achieve optimal outcomes while keeping costs at the lower end of the range?
In the world of health insurance, carve-out contracts are a common tool used to manage the high costs of specialties, such as organ transplants, oncology, and cell and gene therapies. These agreements, often negotiated between insurers and specialized networks or providers, allow for the separation of condition-related services from standard coverage, offering predictable pricing for insurers. However, even with these contracts in place, the phenomenon of Simpson’s Paradox can still lead to significant misinterpretations of cost data, potentially skewing contract terms, repricing operations, and reimbursement methodologies, leading to unintended financial consequences.

What are Carve-Out Contracts?
A carve-out is a contractual arrangement in which a specific set of services, typically related to expensive procedures like organ transplants, is excluded from the general healthcare benefits plan and thus reimbursed separately. This allows health insurers to control the costs of these high-risk, high-cost procedures while giving providers more predictable payments for the services they deliver.
Carve-out contracts often cover:
- Surgical procedures associated with the condition
- Pre-administration evaluations, including things like donor or treatment matching processes
- Post-operative care and immunosuppressive medication management
- Complication management, including hospital readmissions or extended stays
While carve-outs provide financial predictability, the accuracy of the data used to develop these contracts is crucial. If cost trends are misunderstood, particularly due to Simpson’s Paradox, these contracts can be mispriced or fail to adequately cover high-cost patient groups, leading to financial losses for insurers or inadequate care for patients.
What is Simpson’s Paradox?
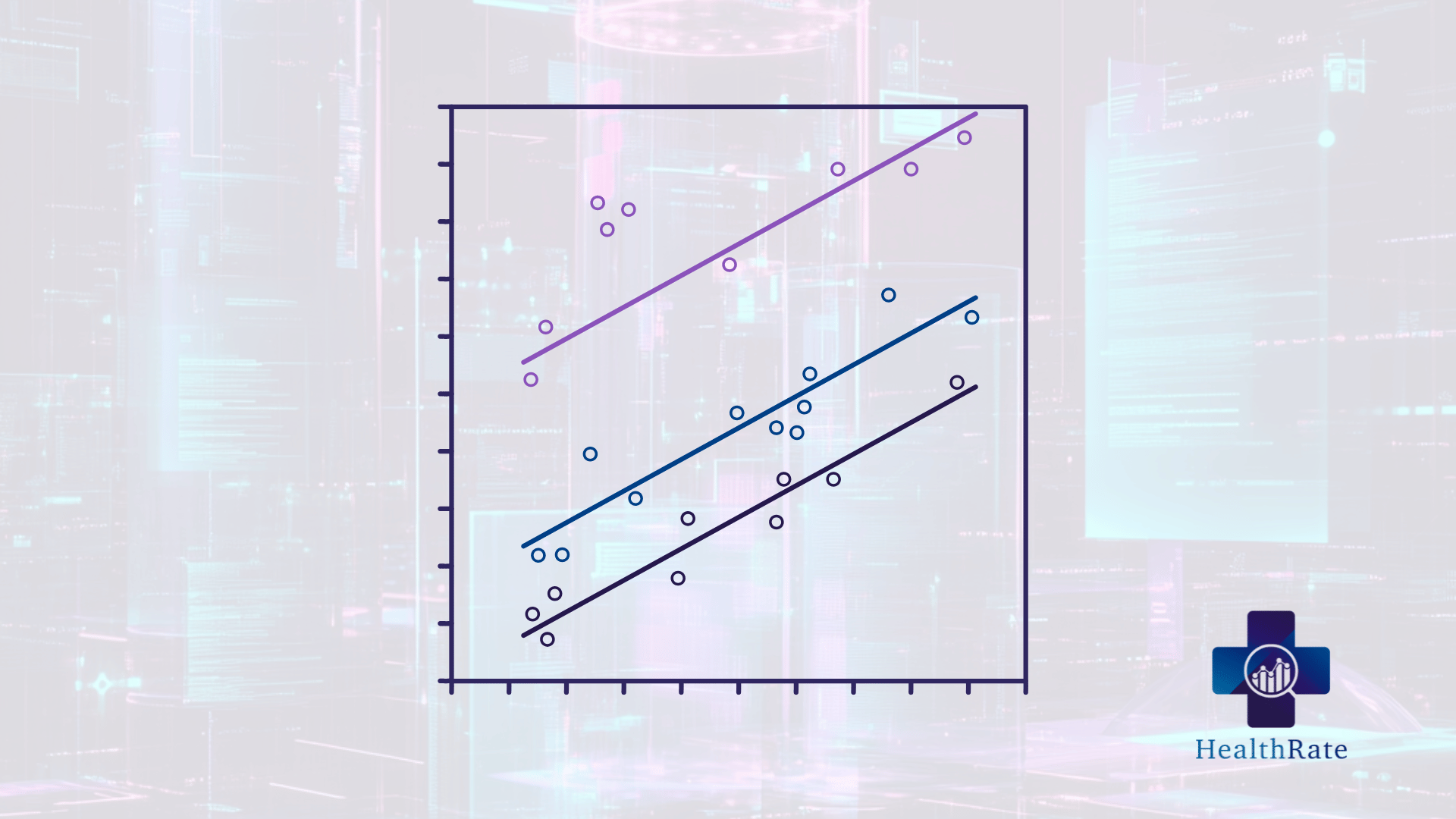
Simpson's Paradox arises when aggregated data masks or reverses the direction of trends observed within subgroups. For instance, in a simplified example, a contract might appear effective for two separate groups of patients, but when data from both groups is combined, the contract could appear ineffective or even financially harmful. This paradox often emerges when there are lurking variables or confounding factors that influence the outcome, leading to erroneous interpretations if not properly accounted for.
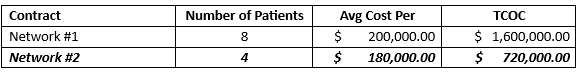
Consider the following contract comparisons:
When contract terms are considered in aggregate the initial conclusion is Network #1 is the most cost-effective.
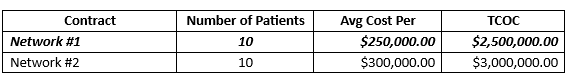
However, when network contracts are divided into two subgroups based on confounding variables, Simpson’s Paradox is demonstrated.
Subgroup A:
Subgroup B:
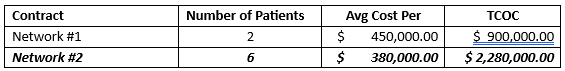
Network #2 has a lower average cost in both subgroup A and subgroup B. Even though Network #2 performs better in both subgroups, the aggregate data suggests that Network #1 is cheaper overall. This is Simpson’s Paradox in action.
This issue frequently arises when analyzing carve-out contracts in aggregate, such as during an annual rate-setting exercise. Before HealthRate, conducting a detailed, case-by-case analysis was simply too complex and costly for most organizations to perform.
The Consequences are Substantial
In healthcare claims analysis, costs are driven by various factors such as demographics (age, gender, socio-economic status), comorbidities, the types of procedures involved, and geographic location. Aggregating data across these variables without recognizing underlying subgroups can produce distorted results, impacting financial performance per case from as little as $50,000 to several million dollars on catastrophic cases.
When Simpson’s Paradox is ignored in healthcare cost analysis, several adverse outcomes can result:
1. Misallocation of Resources: Payers or providers might divert resources to seemingly cost-effective treatments that, when analyzed more granularly, are not actually driving down costs in key patient subgroups. This could result in less effective and more expensive care for high-risk patients.
2. Inaccurate Risk Adjustment: Risk adjustment models are crucial for comparing healthcare provider performance and patient outcomes. If healthcare claims are pooled without adjusting for confounding variables (e.g., age, chronic conditions), the models might over- or under-compensate for risk, leading to skewed reimbursement strategies.
3. Policy Missteps: Healthcare policies aimed at reducing costs or improving outcomes might backfire if they are based on aggregated data that hides subgroup trends. For example, efforts to encourage a specific treatment protocol based on overall cost savings could be ineffective—or worse, harmful—if the protocol is only beneficial in select subpopulations.
4. Reimbursement Models: Health insurers develop reimbursement models based on expected costs. Simpson’s Paradox can distort these models, leading to underpayment or overpayment. For example, suppose older, sicker patients drive higher costs but their data is averaged with healthier patients. In that case, the insurer might fail to fully compensate providers for the true cost of treating high-risk individuals or overcompensate for low-severity individuals.
5. Inadequate Stop-Loss Provisions: Carve-out contracts often include stop-loss provisions that cap insurers' financial liability when transplant costs exceed a certain threshold. If Simpson’s Paradox is at play, and costs are underestimated due to aggregated data, these thresholds may be set too low, leaving risk partners with greater exposure than anticipated.
6. Risk Pooling Challenges: Inaccurate cost data can lead to poor risk pooling in transplant carve-out agreements. Suppose the risk pool is based on aggregated data that doesn’t accurately reflect the complexity of high-risk cases. In that case, insurers may face higher-than-expected claims, jeopardizing the financial sustainability of the contract.
Preventing Misinterpretation: A Call for Sophisticated Data Analytics and Granular Network Evaluation
To mitigate the effects of Simpson’s Paradox, healthcare organizations must adopt more sophisticated data analysis techniques that disaggregate data and adjust for confounding variables. Ideally utilizing toolsets and processes that utilize:
1. Multivariate Analysis: Use statistical models that account for multiple variables simultaneously to isolate the true effect of a particular treatment, intervention, and network contract. By controlling for confounders, the analysis can reveal insights that would be obscured in a simple comparison.
2. Stratification: Break down healthcare claims data by relevant factors such as age, severity of illness, and other demographic variables. This will ensure that comparisons are made between similar groups, avoiding aggregation that hides underlying trends.
3. Scenario-Based Forecasting: In addition to group analysis, contracts can be designed and evaluated with scenario-based forecasting to account for “what if” cases. Insurers can model potential high-cost scenarios, such as patients with complications or extended care needs, and include contingency provisions in the contract. This ensures that underperforming subgroups can be covered without financial strain.
4. Stop-Loss Provisions: Including well-structured stop-loss provisions in the contract can help mitigate financial risk when certain subgroups significantly exceed average costs. By setting appropriate stop-loss thresholds, insurers and providers can share the burden when high-cost subgroups require care that exceeds typical cost expectations.
5. Longitudinal Data Tracking: The costs of specialties such as organ transplants, oncology, and cell and gene therapies don’t end with the procedure. Insurers need to track claims over the long term, capturing the entire patient journey, including follow-up care and the management of any complications. By focusing on long-term outcomes, insurers can develop more accurate cost estimates and better understand the overall value of each network contract.
6. Granular Reimbursement Models: Use granular reimbursement structures that distinguish between different levels of billing. For instance, contracts can include tiered payments based on the severity of the patient’s condition or the expected cost of post-operative care, ensuring that providers are fairly compensated for treating more complex cases.
Conclusion: The High Stakes of Accurate Data Interpretation and Network Selection
In the world of healthcare claims, understanding the true costs of organ transplants is vital for creating sustainable health insurance models that support both patients and providers. Simpson’s Paradox poses a significant challenge in this context, as it can obscure the real cost drivers and lead to misguided conclusions. Health insurers, employers, and providers alike must adopt advanced data analytics methodologies to avoid the trap of oversimplified analysis, ensuring that reimbursement policies are fair, data-driven, and capable of supporting the high-stakes world of specialty carve-out contracting.
Ultimately, by addressing the nuances of network contracts/reimbursement models, insurers can offer better coverage, improve patient outcomes, and ensure a more sustainable approach to financing life-saving procedures.
About the Authors:
Tim Michaels, CEO & Co-Founder at HealthRate | LinkedIn
Michael Hill, Managing Principal, Healthcare Business Consulting at EPAM Systems, Inc.| LinkedIn
*1 - https://pmc.ncbi.nlm.nih.gov/articles/PMC5524376/ “The Changing Financial Landscape of Renal Transplant Practice: A National Cohort Analysis”.
Manage Your Risks Effectively
Try HealthRate today and simplify risk management.